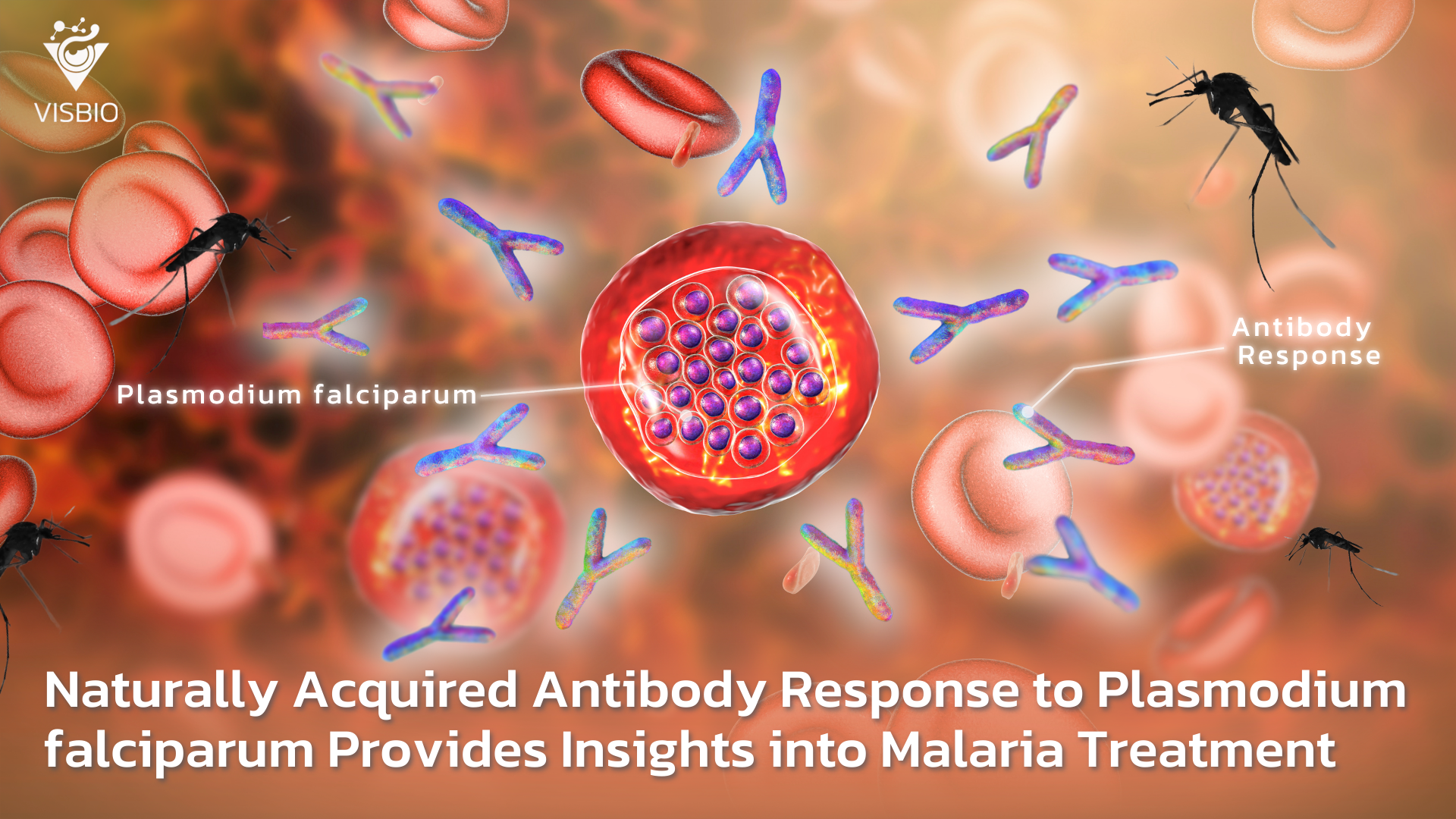
Malaria remains a global health crisis, particularly in regions with high transmission rates, where it causes significant morbidity and mortality. Despite decades of efforts, the disease continues to evade complete eradication, largely due to the adaptive capabilities of Plasmodium falciparum, the most lethal malaria parasite. Recent research has highlighted the role of naturally acquired immunity in shaping innovative malaria treatment and prevention strategies. This study focuses on how antibody responses to specific parasite proteins can provide critical insights for advancing malaria therapies and vaccines.
In malaria-endemic regions, individuals who survive repeated infections often develop partial immunity, which reduces disease severity but rarely provides sterilizing immunity. This immunity is driven by antibodies targeting the surface proteins of the parasite, particularly those expressed during its blood-stage lifecycle. The study explores these naturally acquired antibodies to identify key antigens that could serve as therapeutic or vaccine targets.
Key Findings at a Glance
| Aspect | Findings |
| Antigens Identified | MSP-1, MSP-2, AMA-1, and PfEMP1 were major targets of naturally acquired antibodies. |
| Antibody Longevity | Responses to MSP-1 and MSP-2 persisted longer than other antigens. |
| Breadth of Response | Broader responses correlated with better protection against severe malaria. |
| Correlates of Protection | High levels of IgG antibodies to PfEMP1 reduced the risk of severe malaria. |
| Potential Vaccine Candidates | AMA-1 and MSP-1 show the strongest promise for inclusion in multi-antigen vaccines. |
The study provides a comprehensive overview of the immune response to Plasmodium falciparum, identifying critical antigens such as MSP-1, MSP-2, AMA-1, and PfEMP1 as primary targets of naturally acquired antibodies. Notably, individuals with broader antibody responses exhibited better protection against severe malaria, highlighting the importance of targeting multiple antigens. Among these, AMA-1 and MSP-1 emerged as the most promising vaccine candidates due to their robust and sustained immune responses. Additionally, high levels of IgG antibodies to PfEMP1 correlated with reduced disease severity, underscoring its role in future therapeutic strategies.

The Lifecycle of Malaria Parasite and Immune Evasion
Plasmodium falciparum is a master of immune evasion. During its complex lifecycle, it shifts between liver and blood stages, expressing different proteins to avoid detection. The blood stage, where the parasite invades and multiplies within red blood cells, is particularly critical as it is responsible for the clinical manifestations of malaria, such as fever, anemia, and severe complications.
Key findings from the study reveal:
- Surface Antigens as Key Targets: Proteins such as MSP-1, MSP-2, and AMA-1 play a crucial role in parasite invasion and survival, making them prime targets for antibody-mediated neutralization.
- PfEMP1 and Disease Severity: This protein, expressed on infected red blood cells, mediates cytoadherence, leading to complications such as cerebral malaria. Antibodies targeting PfEMP1 were shown to mitigate these severe effects.

The Promise of Multi-Antigen Vaccines
Single-antigen vaccines have shown limited success due to the parasite’s ability to mutate and evade immune detection. The study advocates for a multi-antigen vaccine approach, combining antigens like AMA-1, MSP-1, and PfEMP1 to elicit broad and durable immune responses. Such a strategy could mimic the natural immunity observed in individuals living in endemic regions, offering better protection against severe malaria.
Broader Implications for Malaria Research and Control
The insights gained from naturally acquired immunity extend beyond vaccine development. They also inform strategies for:
- Therapeutic Antibodies: Harnessing monoclonal antibodies targeting PfEMP1 to prevent severe malaria.
- Serological Tools: Using antibody levels to assess exposure and immunity in populations, aiding in malaria surveillance and control programs.
- Personalized Medicine: Identifying individuals at higher risk of severe disease based on their antibody profiles and tailoring interventions accordingly.

How This Research Opens Doors to New Business Innovations
The findings from this study present significant opportunities for businesses in the biotechnology, pharmaceutical, and diagnostics sectors. Companies can leverage this research to develop next-generation malaria interventions that are not only effective but also economically viable.
- Vaccine Development:
– Multi-antigen vaccines targeting AMA-1, MSP-1, and PfEMP1 could revolutionize malaria prevention.
– Collaboration with endemic regions to conduct clinical trials ensures global health impact and market access. - Therapeutic Antibodies:
– Development of monoclonal antibodies against PfEMP1 to treat severe malaria cases.
– Marketing these therapies as adjuncts to traditional antimalarial drugs. - Diagnostics and Surveillance Tools:
– Serological tests based on antibody responses to MSP-1 and AMA-1 for monitoring population-level immunity.
– Rapid diagnostic kits that combine parasite detection with immunity assessment. - Public-Private Partnerships:
– Engaging governments and international health organizations to scale up production and distribution of vaccines and therapies.
Shaping the Future of Malaria Control
The study’s findings represent a crucial step forward in understanding and combatting malaria. By leveraging naturally acquired immunity, researchers and companies alike can pave the way for innovative interventions that reduce disease burden and save lives. As the world moves closer to malaria elimination goals, the integration of antibody-based strategies will play a pivotal role in shaping a healthier future.
Partner with Us for Innovative Malaria Solutions
Are you ready to invest in next-generation malaria vaccines, therapeutics, or diagnostics? Collaborate with us to translate cutting-edge research into impactful products that address one of the world’s most pressing health challenges. Contact us for a free consultation to explore how your business can contribute to malaria elimination.
About the Author:
Associate Professor Dr. Kiattawee Choowongkomon is a leading researcher in infectious disease immunology and natural product drug discovery, with extensive experience in developing therapeutic solutions against malaria and other tropical diseases. His work focuses on bridging the gap between basic research and clinical application to create effective treatments.
About the Research:
This study, “Acquisition of Naturally Acquired Antibody Responses to Plasmodium falciparum Provides Insights into Malaria Treatment and Prevention,” was published in Malaria Journal (2023). DOI: 10.1186/s12936-023-04567-2. It highlights the role of naturally acquired immunity in identifying vaccine and therapeutic targets for malaria.